Table of Contents
More than 14 million older adults in the United States fall each year, according to the Centers for Disease Control and Prevention (CDC). Unfortunately, accidental falls are the primary cause of injury and injury deaths for older adults.
The aftermath of a fall can also take a significant toll on caregivers, adding to feelings of stress and burnout.
“Caregivers are very focused on the well-being and safety of the person they are taking care of. When a fall occurs it can potentially evoke a range of emotions,” says Iris Waichler, a medical social worker and patient advocate for 40 years.
“There can be feelings of guilt for the caregiver if they were not present at the time of the fall or if they were present and could not stop it,” she adds.
The World Health Organization (WHO) labels falls as a major public health issue. Worldwide, falls are the second leading cause of unintentional injury deaths. In 2022 alone, more than 3,000 fatal falls each month occurred in adults 65 and older, with a total of 40,923 fatal fall injuries in 2022.
Why falls matter
Many of the statistics in this article focus on the physical outcomes of falls, such as injury, hospitalization, and even death. But falls and the fear of falling also impact our mental health.
“Once a fall has occurred, there is underlying fear and anxiety that it can happen again, especially if the cause of the fall is related to a medical or physical condition,” says Waichler.
“It may cause feelings of fear of another fall, a loss of independence, or concern about other related injuries. The concerns of another falling episode can create a fear of going out alone. This can also lead to isolation and loss of self-confidence,” she says.
According to a 2020 study, both single and recurrent falls can lead to depression, while recurrent falls may cause sleep disorders and stress.
The HelpGuide Handbook Team created this resource to address how falls affect our physical and mental health.
Fall prevention and awareness is one of the most important ways to address this health crisis. In addition to reviewing the latest research on older adult falls, the Handbook Team spoke with health care experts about common fall prevention strategies and resources.
Fall statistics
Understanding the causes and outcomes of falls can help us take the necessary precautions to prevent falls and ensure that proper assistance is available when needed.
How falls happen
About 3 million older adults are treated for fall injuries in emergency departments each year, according to the CDC.
There isn’t comprehensive national data on how falls happen or the most likely locations of falls. The Handbook Team reviewed multiple studies and systematic reviews to find this anecdotal information. While the below information is exclusive to each study, it gives us a broader sense of fall patterns, risk factors, and fall locations.
A 2014 study reviewed the outcomes of nearly 1,200 falls reported by 328 study participants:
- About 74 percent of falls occurred indoors, while 26 percent of falls happened outside.
- Falls in the bathroom were the most likely to result in injury compared to other rooms in the home.
- One-third of falls were due to tripping or slipping.
This 2020 analysis reviewed patterns and outcomes of falls resulting in emergency room visits in 2015. It revealed the following:
- The majority of falls occurred in a home setting, with the bedroom, bathroom, and stairs the most common locations of falls.
- More falls occurred in the bedroom for adults 85 years and older compared to adults 65–84 years old.
- A higher percentage of emergency room visits for adults 65–74 years old resulted from falls on the stairs.
An overwhelming majority of older adults fall indoors compared to outdoors, with a home setting the most common location for falls.
A 2019 analysis surveying community-dwelling older adults for four years revealed the following:
- Sixty-two percent of 371 reported falls happened indoors.
- Bedrooms were the most common spot of in-home falls.
- Loss of balance, slipping, or tripping were the most common reasons for falls, followed by uneven floors and navigating steps or stairs.
The above studies focus on community-dwelling older adults. “Community-dwelling” simply means they live in a home setting as opposed to an institutional setting like a nursing home or hospital.
Jeanne Randall, 69, shared that she’s fallen several times, with most of her falls happening in her home. The Rochester, New York, resident has made simple but essential modifications to help reduce her risk of falls.
“I purchased two free-standing half steps with non-slip treads to place in doorways to reduce the height of the step down into my family room,” she says. “My son-in-law installed an ADA-compliant railing by the step that steps down into a ceramic tiled area. The other doorway leads to a carpeted area.”
Randall adds that another helpful preventive measure is keeping her floor space clear, especially before going to bed and removing area rugs. She also uses a flashlight to light her path if she gets up in the middle of the night.
Small but impactful habits can create a safer home environment and help prevent future falls.
Cords, rugs, clutter, and pets are common tripping hazards that may cause falls. Remove these hazards by cleaning clutter from the floor, organizing cords, and replacing rugs with non-skid mats (or removing them completely). If you have a pet, check to see where they are before walking. And never step over your furry friend when walking—make them move first.
The large majority of older adults in the United States live in a community setting (more than 90 percent) versus a nursing home (less than 5 percent), so we didn’t focus on many studies outside of community-dwelling settings.
Sadly, nursing home residents fall at twice the rate of older adults not living in nursing homes, according to a report by the CDC. This report also reveals the following:
- About 50–75 percent of nursing home residents fall each year.
- Residents are likely to fall more than once, with most averaging 2.6 falls per person each year.
- About 10–20 percent of nursing home falls cause serious injuries, while 2–6 percent cause fractures.
- Nearly 1,800 nursing home residents die from falls each year.
Risk factors for falls
Falls are not an inevitable part of aging, and risk factors vary from person to person. A literature review shows the top major fall risks include:
- Poor gait and balance.
- Use of five or more medications.
- Previous fall history.
A 2018 systemic review reveals older adults taking four or more prescription medications daily were up to two times more likely to fall two or more times within a 12-month period.
Other risk factors for falls include:
- Poor eyesight.
- Lower body weakness.
- Cognitive impairment.
- Improper footwear.
Decluttering the home on a consistent basis and securing or getting rid of throw rugs are common fall prevention strategies. Our diet also plays a huge role in fall prevention. Eating vegetables that contribute to bone health and diets with an adequate amount of protein can be helpful. Individuals should always consult with their physicians, dietitians, or nutritionists to receive guidance.
Christina Peoples, a gerontologist based in Greensboro, North Carolina.
Health conditions
Certain health conditions, such as diabetes, thyroid issues, and heart disease, can also increase the risk of falling.
Dementia is another fall risk factor: Research shows fall rates are higher for older adults living with dementia compared to those who don’t have dementia.
Age
Although falls aren’t a natural part of the aging process, our risk of falling does increase with age. More than 30 percent of adults over 65 years old fall each year. The number jumps to 40 percent for adults 85 years and older.
Assigned sex
There is little comprehensive research that supports assigned sex at birth as a fall risk. Traditionally, fall risk data has been gathered according to a gender binary (male and female), and few studies focus on assigned sex as the main risk. The studies that do have small sample sizes.
Fall risks for nursing home residents
Fall risks are slightly different for nursing home residents compared to older adults living in a home setting:
- Top fall risk factors for nursing home residents and hospital patients include history of falls, walking aid use, and moderate disability, according to a systematic review and meta-analysis published in 2013.
- Fall history, impaired activities of daily living (ADL) performance, insomnia, and depression were the top fall risk factors for nursing home residents, according to a systematic review and meta-analysis published in 2023.
Outcomes of falling
Falls can lead to injury, hospitalization, and even death. Fall prevention strategies and awareness are crucial to preventing these severe outcomes.
- Hip fractures, bruises, and head trauma are prevalent injuries from falls. The WHO reports 20–30 percent of older adults who fall in the United States suffer moderate to severe injuries such as bruises, hip fractures, or head trauma.
- The likelihood of a fall resulting in hospitalization increases with age. More than 95,000 older adults are hospitalized each year as a result of a fall injury. The chances of a fall requiring hospitalization doubles between the ages of 65 and 90.
- The number of older adult deaths from falls is increasing. The fall death rate increased by 41 percent from 2012 to 2021 for adults 65 and older.
The financial cost of falls
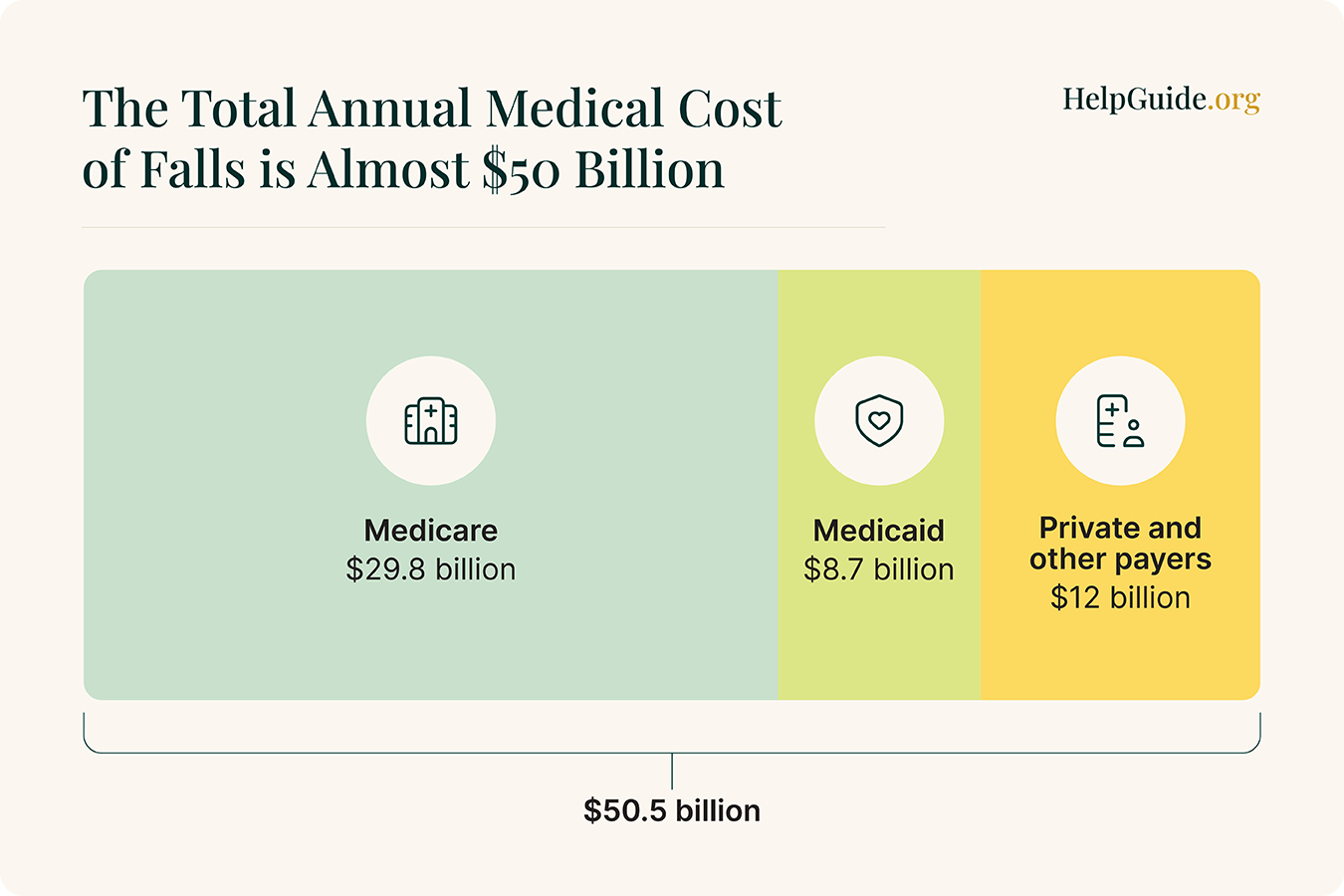
- Falls are an expensive public health issue. Medical costs related to falls are estimated at nearly $50 billion.
- Medicare pays the most fall-related medical costs. Medicare paid about $28.9 billion, Medicaid $8.7 billion, and private and other payers paid $12 billion for nonfatal falls in 2015.
- Lifetime medical costs of falls keep increasing. This cost is projected to increase from $35 billion in 2012 to more than $101 billion in 2030.
Fall statistics by state
Each year, the CDC tracks the percentage of reported older adult falls in every state. According to the most recent data, every state but Illinois reported that at least 20 percent of older adults experienced a fall in 2020.
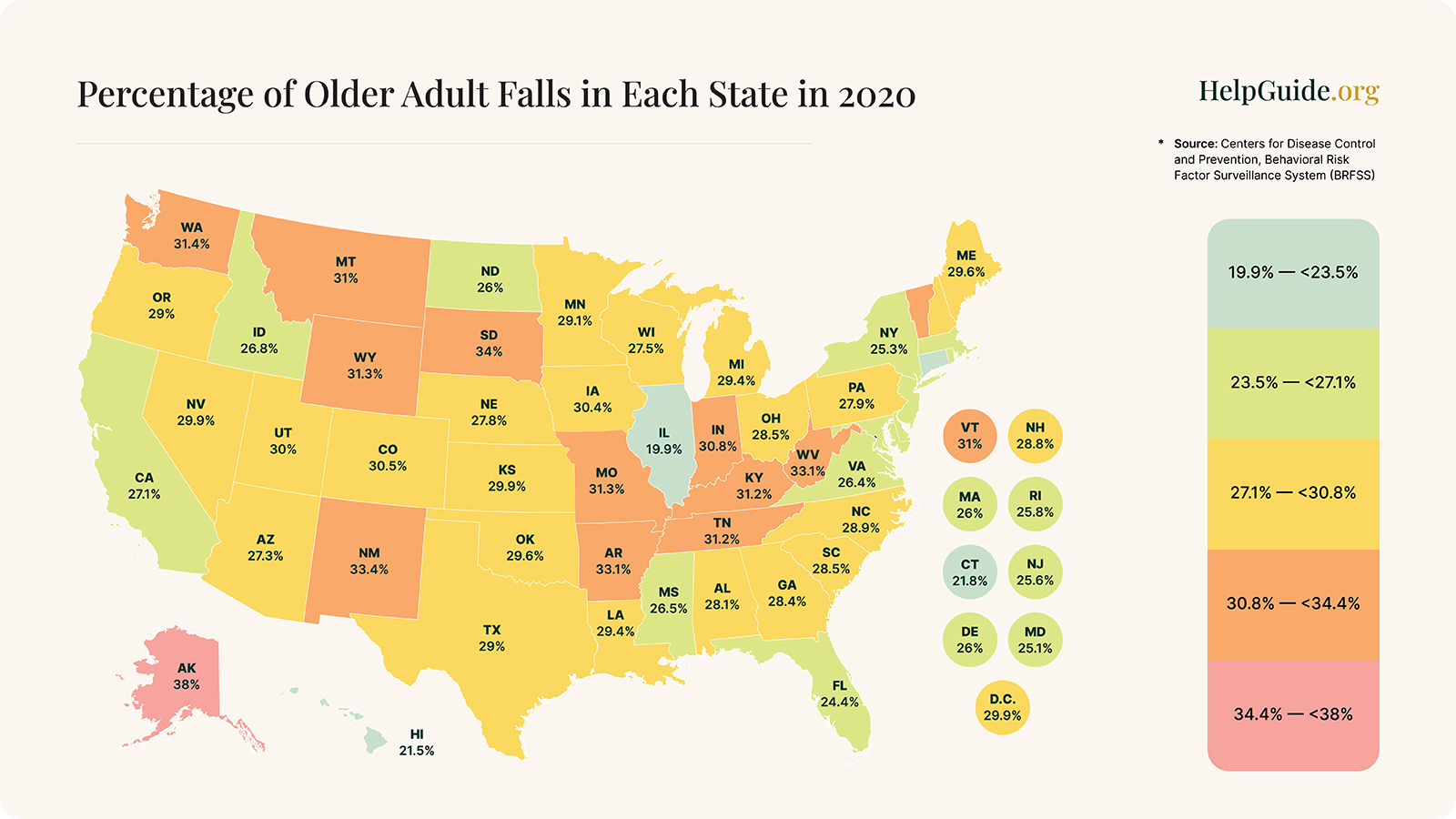
The top three states with the highest percentage of falls:
- Alaska (38 percent).
- South Dakota (34 percent).
- New Mexico (33.4 percent).
The three states with the lowest percentage of falls:
- Illinois (19.9 percent).
- Hawaii (21.5 percent).
- Connecticut (21.8 percent).
Sadly, some older adults die as a direct result of falling. The CDC organizes this data by the fall death rate per 100,000 older adults, with the most recent numbers from 2021.
Top three states with the highest fall death rate for older adults:
- Wisconsin (176.5).
- Minnesota (141.8).
- South Dakota (140.3).
All three states are in the central northern region of the United States. While we can’t make any conclusions about this commonality, we thought this was an interesting observation.
Top three states with the lowest fall death rate for older adults:
- Alabama (30.7).
- New Jersey (31.5).
- California (43.1).
Preventing falls and their outcomes
Unfortunately, injuries and deaths from falls are on the rise: In the United States, fall deaths have increased by 60 percent and emergency room visits due to falls have increased by 20 percent in the last decade, according to the National Safety Council. There has been a significant push for fall prevention in the past few decades to help address fall injuries and fatalities.
Fall Prevention Awareness Week begins on the first day of fall, with many aging and health care organizations promoting prevention strategies like mobility exercises, home modifications, assistive devices, and working with a health care provider.
While this is an excellent initiative, gerontologist Christina Peoples expresses that we need to see more fall prevention awareness year-round—not limited to one week. “The more education about fall prevention shared the better,” she says.
Fall prevention strategies can be divided into two main categories:
- Environmental fall prevention: Adjusting your environment to help reduce fall risks, such as removing tripping hazards and installing assistive devices like grab bars.
- Lifestyle fall prevention: Incorporating health and wellness routines to help reduce fall risks, such as exercise programs to strengthen muscles and improve balance, and eating a well-balanced diet to support healthy aging.
We’ve consolidated common environmental and lifestyle fall prevention tips from the CDC, National Institute on Aging, and WHO below.

Adding railings to stairways, improving slippery pathways, and increasing overhead lighting in the home can reduce the number of falls by 38 percent for older adults with a higher risk of falling, according to a study published in 2023.
“In my experience, the best way to reduce the chances of injury from a fall is to prevent the fall through exercise training and hazard reduction,” says Gerda Maissel, a physician and president at My MD Advisor. “Exercise helps because even if you start to fall, if your muscles contract strongly and quickly, you will fall more safely than if you go straight down.”
Learning your fall risk by undergoing screening is another preventive measure. We spoke with Peoples about balance screening, an assessment tool focusing on a person’s gait, strength, balance, medication usage, fall history, and vision. “These screenings look at how well an individual is able to stand up and walk, and stand up and sit down,” she says. Talk to your doctor about a screening if you think you might have a higher risk for falls.
Medical alert systems don’t prevent falls, but these devices can connect you with help shortly after a fall. The best medical alert systems offer fall detection, which allows the device to automatically contact a 24/7 monitoring center when it detects a fall.
Getting help shortly after a fall helps avoid a “long lie” (lying on the floor after a fall for more than an hour). Pressure sores, dehydration, and an increased risk of death within six to 12 months are potential outcomes of a long lie.
Our final verdict
Falls are a stressful event for the person who has fallen, as well as for their caregivers, family members, and friends. Behind the above statistics and facts, real people are experiencing the physical, mental, and financial effects of falls.
Your health care provider and local organizations, such as an area agency on aging or your region’s council on aging, are valuable resources for fall prevention programs.
If you’re a caregiver helping implement fall prevention strategies, remember this may be a difficult adjustment for your care recipient.
“Just the fact that interventions are needed to reduce their risk of falling is an emotionally uncomfortable reminder that they are aging,” says Maissel. “I try to be very sensitive to that internal possibility and avoid assuming that interventions are going to make someone feel good about themselves.”
“In my experience, the people that feel best about the reduced risk of falling are the family members and caregivers,” she adds. “Those who made changes sometimes feel proud that they are stronger and sometimes feel less fearful.”
- Moreland, B., Henry, A., & Kakara, R. (2020, July 10). Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years – United States, 2012–2018. Centers for Disease Control and Prevention. Link
- Centers for Disease Control and Prevention. (2023, August 10). Fatal injury trends. Link
- World Health Organization. (2021, April 26). Falls. Link
- National Safety Council: Injury Facts. (2021). Older adult falls. Link
- Jo, K. H., Park, J., & Ryu, S. Y. (2020). The effects of mental health on recurrent falls among elderly adults, based on Korean Community Health Survey Data. Epidemiology and Health, 42. Link
- Centers for Disease Control and Prevention. (2023). Facts about falls. Link
- Stevens, J. A., Mahoney, J.E., Ehrenreich, H. (2014). Circumstances and outcomes of falls among high-risk community-dwelling older adults. Injury Epidemiology, 5(2014). Link
- Moreland, B. L., Kakara, R., Haddad, Y.K., Shakya, I., Bergen, G. (2020). A Descriptive Analysis of Location of Older Adult Falls That Resulted in Emergency Department Visits in the United States, 2015. American Journal of Lifestyle Medicine, 15(6), 590–597. Link
- Piau, A., Mattek, N., Duncan, C., Sharma, N., Riley, T., Kaye, J. (2019). The Five W’s of Falls: Weekly Online Health Survey of Community-Dwelling Older Adults: Analysis of 4 Years Prospective Follow-up. The Journals of Gerontology: Series A, 75(5), 946–951. Link
- Toth, M., Martin Palmer, L.A., Bercaw, L.E., Voltmer, H., Karon, S. (2020). Trends in the Use of Residential Settings Among Older Adults: Issue Brief. Office of the Assistant Secretary for Planning and Evaluation. Link
- Centers for Disease Control and Prevention. (2012). Falls in nursing homes. Link
- Ambrose, A., Geet, P., Hausdorff, J.M. (2013). Risk factors for falls among older adults: A review of the literature. Maturitas, 75(1), 51-61. Link
- Ming, Y., and Zecevic, A. (2028). Medications & polypharmacy influence on recurrent fallers in community: a systematic review. Canadian Geriatrics Journal, 21(1). Link
- National Institute on Aging. (2022). Falls and fractures in older adults: causes and prevention. Link
- Okoye, S. M., Fabius, C.D., Reider, L., Wolff, J.L. (2023). Predictors of falls in older adults with and without dementia. Alzheimer’s & Dementia, 19(7), 2888-2897. Link
- Appeadu, M. K., & Bordoni, B. (2023, January). Falls and fall prevention in older adults – StatPearls – NCBI bookshelf. National Library of Medicine. Link
- Deandrea, S., Bravi, F., Turati, F., Lucenteforte, E., La Vecchia, C., Negri, E. (2013). Risk factors for falls in older people in nursing homes and hospitals: A systematic review and meta-analysis. Archives of Gerontology and Geriatrics, 56(3), 407–415. Link
- Shao, L., Shi, Y., Xie, X.-Y., Wang, Z., Wang, Z.-A., & Zhang, J.-E. (2023). Incidence and risk factors of falls among older people in nursing homes: Systematic review and meta-analysis. Journal of the American Medical Directors Association, 24(11), 1708–1717. Link
- World Health Organization. (2021). Falls. Link
- Centers for Disease Control and Prevention: Injury Prevention & Control. (2023). Web-based injury statistics query and reporting system (WISQARS). Link
- Miller, A., Watson, W., Monger, C., Barr, M., Giffin, M., Reid, M. (2011). Prevalence, circumstances and consequences of falls among community-dwelling older people: Results of the 2009 NSW falls prevention baseline survey. New South Wales Public Health Bulletin, 22(3–4). Link
- Centers for Disease Control and Prevention. (2020). Older adult falls data. Link
- Florence, C., Bergen, G., Atherly, A., Burns, E., Stevens, J., Drake, C. (2018). Medical costs of fatal and nonfatal falls in older adults. Journal of the American Geriatrics Society, 66(4), 693–698. Link
- Houry, D., Florence, C., Baldwin, G., Stevens, J., McClure, R. (2016). The CDC Injury Center’s response to the growing public health problem of falls among older adults. American Journal of Lifestyle Medicine, 10(1), 74–77. Link
- Centers for Disease Control and Prevention. (2017). What you can do to prevent falls. Link
- National Institute on Aging. (2022). Preventing falls at home: room by room. Link
- Clemson, L., Stark, S., Pighills, A.C., Fairhall, N.J., Lamb, S.E., Ali, J., Sherrington, C. (2023). Environmental interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews. Link
- Ang, G. C., Lin Low, S., How How, C. (2020). Approach to falls among the elderly in the community. Singapore Medical Journal, 61(3), 116–121. Link
- Wild, D., Nayak, U.S., and Isaacs, B. (1981). How dangerous are falls in old people at home? British Medical Journal (Clinical Research Edition), 282 (6260), 266–268. Link




